Our researchers hold expertise in diverse areas across allied health including rural health, persistent pain, stroke recovery, child health, persistent breathlessness, and health services research.
Interested in participating in our research? Check out our current projects for to see if you are eligible to participate. Interested in what we have accomplished? Check out our research impact case studies, and explore our researchers profiles to see their outputs and other achievements.
Research Impact
New Treatments and their Implementation
-
Translating evidence-based breathlessness intervention services to South Australia
This pilot study evaluated the feasibility and outcomes of translating an evidence-based Breathlessness Intervention Service (BLIS) for people in the local setting with chronic breathlessness associated with COPD.
The BLIS program:

- was feasible, acceptable and accessible
- had a positive impact post-program on lowering distress and perceived threat associated with breathlessness
- participants’ total hospital use was lower in the 12 months after than the 12 months before receiving the program
Watch a video explaining our approach to Breathlessness Intervention Services.
Lead Researcher: A Prof Kylie Johnston
Funding: Medical Research Future Fund through HTSA Rapid Applied Research Translation Grant: 2019
-
ifarmwell

ifarmwell is an online, self-help program, designed based upon what farmers want and what research has shown will help improve farmers’ wellbeing and ability to cope with things beyond their control (e.g. drought).
Hear how ifarmwell made Kym's life easier to live in this video.
Lead Researcher: A/Prof Kate Gunn
Current funding partners: James & Diana Ramsay Foundation, Thyne Reid Foundation, Qantas, Lang Family Foundation, SA Drought Hub
-
Boot Camp: Intensive stroke rehabilitation for arm recovery
Stroke is a leading cause of disability globally. One in four people over the age of 25 will experience a stroke in their lifetime.
 Rehabilitation is needed to help restore movement and reduce disability.
Rehabilitation is needed to help restore movement and reduce disability.There is belief that most recovery happens in the first weeks after stroke, with recovery beyond 3 months unlikely. Here, we dispel that myth, showing large gains are possible with an intensive burst of rehabilitation.
Lead Researcher: Dr Brenton Hordacre
Funding: Hospital Research foundation (2023-24)
-
A Novel Gait Training Technology to Improve Mobility, Health and Wellbeing after Brain and Spinal Cord Injury
People with complex injuries, such as lower-limb amputation, brain and spinal cord injury, frequently identify recovery of functional mobility as a primary rehabilitation goal. Providing sufficient and appropriate walking training can be challenging. Intensity, repetition and salience are key factors in neuroplasticity and motor learning. We tested a novel gait training technology to facilitate greater practice of task specific, mobility training. Ten sessions with the treadmill led improved mobility and reduced sedentary time.

Lead Researcher: Dr Brenton Hordacre
Funding: Lifetime Support Authority (2022-23)
-
The EPIPHA-KNEE Trial: Explaining Pain to Increase PHysical Activity in people with painful KNEE osteoarthritis
Knee osteoarthritis is both common and disabling in middle aged and older adults. Many people with knee osteoarthritis are
 physically inactive. They do not undertake enough activity to maintain their overall health or their knee health. This clinical trial compared two activity-based interventions, delivered by licensed physiotherapists, evaluating clinical effectiveness and cost- effectiveness. The statistical analysis is underway. These findings will help guide what type of treatment should be provided as part of regular clinical practice for people with knee osteoarthritis.
physically inactive. They do not undertake enough activity to maintain their overall health or their knee health. This clinical trial compared two activity-based interventions, delivered by licensed physiotherapists, evaluating clinical effectiveness and cost- effectiveness. The statistical analysis is underway. These findings will help guide what type of treatment should be provided as part of regular clinical practice for people with knee osteoarthritis.Lead Researcher: A/Prof Tasha Stanton
Funding: National Health & Medical Research Council
-
A Virtual Reality cycling intervention to improve exercise experiences in people with osteoarthritis
Exercise is often painful for people with knee osteoarthritis. And for those who are inactive, beginning an activity or exercise regime can seem daunting. This study aimed to test the potential for a new intervention – virtual reality cycling – to improve exercise enjoyment and engagement. The project had 3 stages: first, people with painful knee osteoarthritis and physiotherapists were consulted for their thoughts on the virtual reality bike. The virtual reality bike was tested in the lab and in the clinical environment and iteratively changed based on feedback. Second, the effect of one session of the virtual reality bike was tested in people with painful knee osteoarthritis: people enjoyed the virtual reality bike exercise experience more and worked harder than when cycling without virtual reality. Third, a pilot feasibility randomised controlled trial found that a prolonged virtual reality bike intervention (2x/week over 6 weeks) was safe, had high ratings of perceived acceptability and credibility in people with painful knee osteoarthritis and was successfully provided by physiotherapists in the clinical environment. This promising data suggests that virtual reality cycling may hold merit as a new exercise intervention for people with knee osteoarthritis.
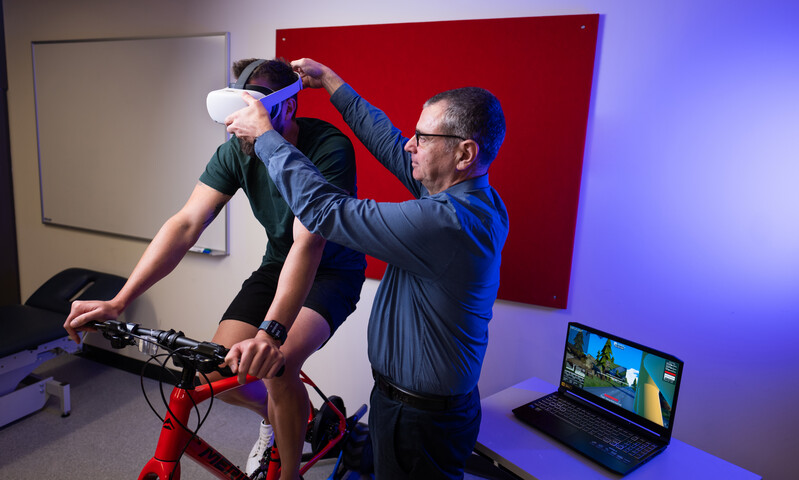
Lead Researcher: Erin MacIntyre
Funding: The Hospital Research Foundation, UniSA Research Themes Investment Scheme
-
Identifying Social factors that Stratify Health Opportunities and Outcomes (ISSHOOs) in Pain Research

The ISSHOOs Project is a multi-stage consensus project that aims to develop the definitive tool by which equity-relevant data will be routinely collected in all pain research. It is an international, inter- disciplinary, key-interest holder engaged project that prioritises patient participation at all stages. The project involves literature reviews, a Delphi study, Consensus Meetings and Focus Groups. The deliverables will be a short ‘minimum data’ tool for use in all pain studies globally, and an extended equity-relevant standardised item set for use in research targeting equity-related matters associated with pain. The final phase of the ISSHOOs project will involve widespread dissemination and endorsement of both tools by peak associations, journals and funding bodies.
Lead Researcher: Dr Emma Karran, Research Fellow, Body in Mind Research Group
Funding: Australian National Health and Medical Research Council Leadership Investigator Grant awarded to Lorimer Moseley (NHMRC ID 1178444). -
Explaining and evaluating breathlessness.
Developing useful explanations for persistent breathlessness is challenging. In people with chronic conditions, multiple
 factors contribute to the experience of persistent breathlessness and this sensation does not have a consistent, proportional relationship with markers of disease severity (e.g., ., pulmonary function, imaging results, oxygenation). We have sought information from health professionals and people living with breathlessness considered to be important to include or avoid within explanations for persistent breathlessness. We have created a standardised process for assessing the helpfulness and understandability of explanations and are currently ‘field testing’ several written explanations for persistent breathlessness.
factors contribute to the experience of persistent breathlessness and this sensation does not have a consistent, proportional relationship with markers of disease severity (e.g., ., pulmonary function, imaging results, oxygenation). We have sought information from health professionals and people living with breathlessness considered to be important to include or avoid within explanations for persistent breathlessness. We have created a standardised process for assessing the helpfulness and understandability of explanations and are currently ‘field testing’ several written explanations for persistent breathlessness.Lead Researcher: Prof Marie Williams
-
Measuring disrupted body perception in people with knee osteoarthritis
People with knee osteoarthritis sometimes report that their knee feels ‘wrong’ to them, that
 they have a hard time knowing where it is in space and that they need to pay close attention to it when moving. We created a new questionnaire, called the Fremantle Knee Awareness Questionnaire (FreKAQ) to capture this aspect of disrupted body perception. We found that the questionnaire was reliable and had adequate measurement properties. We also found that greater impairment in body perception (higher FreKAQ scores): i) were associated with a more severe clinical phenotype in people with painful knee osteoarthritis; ii) predicted non-response to exercise interventions; and iii) predicted development of chronic post-surgical pain after total knee replacement surgery. This clinically friendly resource can be used to evaluate the presence of impaired body perception in people with knee osteoarthritis and may help guide which patients may require treatment targeting sensory and motor processing.
they have a hard time knowing where it is in space and that they need to pay close attention to it when moving. We created a new questionnaire, called the Fremantle Knee Awareness Questionnaire (FreKAQ) to capture this aspect of disrupted body perception. We found that the questionnaire was reliable and had adequate measurement properties. We also found that greater impairment in body perception (higher FreKAQ scores): i) were associated with a more severe clinical phenotype in people with painful knee osteoarthritis; ii) predicted non-response to exercise interventions; and iii) predicted development of chronic post-surgical pain after total knee replacement surgery. This clinically friendly resource can be used to evaluate the presence of impaired body perception in people with knee osteoarthritis and may help guide which patients may require treatment targeting sensory and motor processing.Lead researchers: A/Prof Tasha Stanton & Prof Tomohiko Nishigami (Prefectural University of Hiroshima).
Funding: Arthritis Australia
Understanding Health Conditions and Care Pathways to Improve Care
-
Making sense of breathlessness
Persistent, disabling breathlessness is an everyday experience for many people living with heart, lung,
 and neuromuscular conditions. How people ‘make sense’ of this unpleasant sensation was explored with twenty-one community-dwelling individuals living with varying levels of breathlessness-related impairment. People made sense of breathlessness based on their personal experience (beliefs about the underlying causes /contributors) informed by health professionals/internet. Specific words and phrases about breathlessness were identified as contributors to helpful or non-helpful breathlessness beliefs. This information will be used to develop more helpful breathlessness education.
and neuromuscular conditions. How people ‘make sense’ of this unpleasant sensation was explored with twenty-one community-dwelling individuals living with varying levels of breathlessness-related impairment. People made sense of breathlessness based on their personal experience (beliefs about the underlying causes /contributors) informed by health professionals/internet. Specific words and phrases about breathlessness were identified as contributors to helpful or non-helpful breathlessness beliefs. This information will be used to develop more helpful breathlessness education.Lead Researcher: Becky Burgess (Master of Research)
Funding: Australian government Research Training Program scholarship (stipend and fee waiver).
-
Evidence for a Window of Enhanced Plasticity in the Human Motor Cortex Following Ischemic Stroke
Stroke is a global leading cause of adult disability. Recovery occurs through neuroplasticity, the ability of the brain to change. A
 nimal models indicate there may be a brief period after stroke where the brain capacity for neuroplasticity is increased. This critical time appears highly sensitive to rehabilitation training.
nimal models indicate there may be a brief period after stroke where the brain capacity for neuroplasticity is increased. This critical time appears highly sensitive to rehabilitation training.
In this study, we evaluated neuroplasticity in humans to discover evidence of a similar increase in neuroplasticity within weeks of stroke. Delivery of rehabilitation during this sensitive period appears to offer great hope for accelerating recovery.Lead Researcher: Dr Brenton Hordacre
Funding: National Health and Medical Research Council -
Exploring Parent and Educator Perspectives on Nature Play in Early Childhood Settings: Challenges, Opportunities, and the Role of Adults
Nature play is growing in popularity, with many early childhood settings transforming their outdoor play
 environments to incorporate more natural elements. Current research highlights the benefits of engaging in unstructured nature play for children’s health and development. However, the experiences of parents and educators, who play a crucial role in implementing nature play, are less understood. This study aimed to address this knowledge gap by exploring parent and early childhood educator (ECE) perspectives to gain an understanding about their experiences with nature play. Using a qualitative descriptive approach, semi-structured in-person and telephone interviews were conducted with 18 ECE and 13 parents across four early childhood centres (from various socio-economic regions) across metropolitan Adelaide, South Australia during 2019–2020. The findings suggest that parents and ECEs may need additional resources and guidance on how to engage with nature play and how to overcome barriers within early childhood settings and the home environment.
environments to incorporate more natural elements. Current research highlights the benefits of engaging in unstructured nature play for children’s health and development. However, the experiences of parents and educators, who play a crucial role in implementing nature play, are less understood. This study aimed to address this knowledge gap by exploring parent and early childhood educator (ECE) perspectives to gain an understanding about their experiences with nature play. Using a qualitative descriptive approach, semi-structured in-person and telephone interviews were conducted with 18 ECE and 13 parents across four early childhood centres (from various socio-economic regions) across metropolitan Adelaide, South Australia during 2019–2020. The findings suggest that parents and ECEs may need additional resources and guidance on how to engage with nature play and how to overcome barriers within early childhood settings and the home environment.Lead Researcher: PhD candidate Mrs Kylie Dankiw
Funding: Mrs Dankiw supported by the Government of Australia Research Training Program Scholarship
-
Lung function surveillance in the South Australian Metropolitan Fire Service (SAMFS)
This project involved two studies. The first, analysed 6 rounds of SAMFS lung function data collected between 2007 and 2019, using a new method that separated firefighters into groups based their lung function trajectory. In the second study, SAMFS firefighters were interviewed to determine their experiences and attitudes towards participating in lung function surveillance. This information will help guide assessment of lung function to better inform management.
Lead Researcher: Cathy Pendergrast, MRes CRFS ACP, Senior Medical Scientist
Funding: University of South Australia Firefighter Lung Function Scholarship provided by the SAMFS and the Australian Government Research Training Program (2021-22)
-
The predictors of hospitalisation for low back pain – can we improve the delivery of healthcare for people with low back pain?
Increasing numbers of people present to hospital emergency departments with low back pain. The majority can be safely managed in community health settings as per clinical guidelines. In Australian hospitals, there is overreliance on diagnostic imaging, medication prescriptions – especially opioids, and hospital admissions. This is at great expense without always improving patient outcomes. Given the pressures on hospital systems, there is need to better understand the factors that lead to hospitalisation for low back pain, so that we can inform more appropriate healthcare delivery. To explore this research question, our team has summarised the known literature on the topic, audited data on hospitalisations for low back pain from South Australian public hospitals, interviewed patients with lived experiences of being admitted for low back pain, and analysing the impact of a hospital avoidance service as an alternative to an emergency department for people with low back pain.
Lead Researcher: Joseph Orlando, HDR student
Funding:
- Government of Australia Research Training Program Scholarship
- The Hospital Research Foundation, ASHO Allied Health Research Collaboration, 2021
- Allied & Scientific Health Office Seed Funding, 2023 & 2024
- Hospital Services Charitable Gifts Board 2023 & 2024
-
Exploring Allied Health Models of Care for Children with Developmental Health Concerns, Delays, and Disabilities in Rural and Remote Areas
Children in rural and remote areas are more vulnerable than their metropolitan counterparts. A
 ccess to appropriate healthcare is essential for children’s healthy development. This is lacking in rural and remote areas, impacting health outcomes. Despite efforts to improve access for these communities, to date, no review has systematically mapped the literature on allied health models of care for children with developmental needs. Multiple models of care are currently in operation for children with developmental needs in rural and remote areas and appear to improve the quality of care. Due to complexities within, and limitations of, the evidence base, it is unclear if one model of care is superior to another. This review provides a basis for further research to explore why some models may be more effective than others.
ccess to appropriate healthcare is essential for children’s healthy development. This is lacking in rural and remote areas, impacting health outcomes. Despite efforts to improve access for these communities, to date, no review has systematically mapped the literature on allied health models of care for children with developmental needs. Multiple models of care are currently in operation for children with developmental needs in rural and remote areas and appear to improve the quality of care. Due to complexities within, and limitations of, the evidence base, it is unclear if one model of care is superior to another. This review provides a basis for further research to explore why some models may be more effective than others.Lead Researcher: Georgia Gosse, PhD Candidate
Funding: Supported by the Government of Australia Research Training Program Scholarship and Enterprise Research Scholarship.



