16 August 2021
They’re roughly the same size as a coronavirus particle, and 1000 times smaller than a human hair, yet newly engineered nanoparticles developed by scientists at the University of South Australia, are punching well above their weight when it comes to treating drug-resistant fungal infections.
Created in partnership with Monash University, the new nanobiotechnology (called ‘micelles*’), has a remarkable ability to battle one of the most invasive and notoriously resistant fungal infections – Candida albicans.
It’s a timely finding, especially given the significant rise of dangerous fungal infections in hospitals with countries overrun by COVID-19.
Candida albicans is an opportunistic pathogenic yeast that is extremely dangerous to people with compromised immune systems, particularly those in a hospital setting. Found on many surfaces, Candida albicans is notorious for its resilience to anti-fungal medicines. It is the most prevalent cause of fungal infections worldwide and can cause serious infections that can affect the blood, heart, brain, eyes, bones, and other parts of the body.
Senior investigator, UniSA’s Professor Clive Prestidge says the new polymer-based micelles could revolutionise current anti-fungal medicines.
“Managing and treating invasive fungal infections is particularly challenging because so many fungal biofilms are resistant to contemporary antifungal drugs,” Prof. Prestidge says.
“Fungal biofilms are surface-loving microbials that thrive on implanted devices such as catheters, prostheses and heart valves, making the presence of these devices a major risk factor for infection.
“In places like India – which has nearly 40,000 new COVID-19 infections every day – hospital resources are severely stretched, leaving healthcare workers are not only battling COVID-19, but also dealing with complacency and fatigue.
“The unfortunate result is that infection control practices have deteriorated, putting patients on mechanical ventilation at greater risk of developing bacterial or fungal infections.
“As fungal biofilms tend to seed recurrent infections, finding ways to break and beat the infection cycle is critical, especially now.
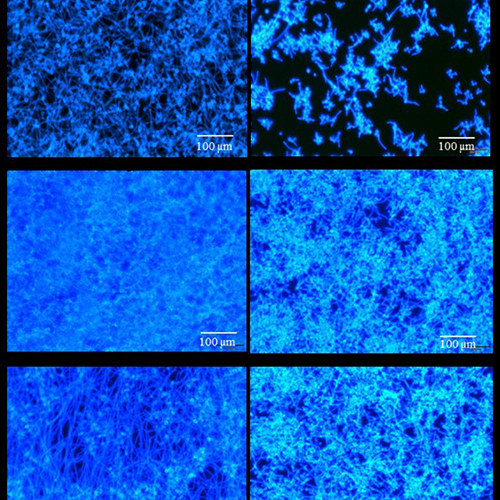
“Our research has identified and developed smart micelles that have the ability to break down single and multi-species biofilms to significantly inhibit the growth of Candida albicans, one of the most virulent fungal species.
“We estimate that the new micelles could improve the efficacy of anti-fungal medicines by 100-fold, potentially saving the lives of millions of people worldwide.”
Dr Nicky Thomas, co-investigator, says the new micelles present a breakthrough for treating invasive fungal infections.
“These micelles have a unique ability to solubilize and entrap a range of important antifungal drugs to significantly improve their performance and efficacy”.
“This is the first time that polymer-based micelles have been created with intrinsic capabilities to prevent fungal biofilm formation.
“As our results already show that the new micelles will remove up to 70 per cent of infection, this could be a real game changer for treating fungal diseases.”
Notes to editors:
* Micelles are made of lipid molecules that arrange themselves in a spherical form in aqueous solutions. They both attract and repel liquids, making them particularly well suited for drug delivery.
The two key papers are available online:
Albayaty, Y.N., Thomas, N., Ramírez-García, P.D. et al. Polymeric micelles with anti-virulence activity against Candida albicans in a single- and dual-species biofilm. Drug Deliv. and Transl. Res. 11, 1586–1597 (2021).
Albayaty Y.N., Nicky Thomas N., Ramírez-García P.D., et al., pH-Responsive copolymer micelles to enhance itraconazole efficacy against Candida albicans biofilms, J. Mater. Chem. B, 2020, 8, 1672-1681
…………………………………………………………………………………………………………………………
Media contact: Annabel Mansfield M: +61 417 717 504 E: Annabel.Mansfield@unisa.edu.au
Contacts for interview: Professor Clive Prestidge E: Clive.Prestidge@unisa.edu.au
Dr Nicky Thomas E: Nicky.Thomas@unisa.edu.au




